WO1994008237A1 - Method and apparatus for direct spectrophotometric measurements in unaltered whole blood - Google Patents
Method and apparatus for direct spectrophotometric measurements in unaltered whole blood Download PDFInfo
- Publication number
- WO1994008237A1 WO1994008237A1 PCT/US1993/009154 US9309154W WO9408237A1 WO 1994008237 A1 WO1994008237 A1 WO 1994008237A1 US 9309154 W US9309154 W US 9309154W WO 9408237 A1 WO9408237 A1 WO 9408237A1
- Authority
- WO
- WIPO (PCT)
- Prior art keywords
- vector
- radiation
- sample
- concentrations
- scattering
- Prior art date
Links
Classifications
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N21/00—Investigating or analysing materials by the use of optical means, i.e. using sub-millimetre waves, infrared, visible or ultraviolet light
- G01N21/17—Systems in which incident light is modified in accordance with the properties of the material investigated
- G01N21/25—Colour; Spectral properties, i.e. comparison of effect of material on the light at two or more different wavelengths or wavelength bands
- G01N21/31—Investigating relative effect of material at wavelengths characteristic of specific elements or molecules, e.g. atomic absorption spectrometry
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N33/00—Investigating or analysing materials by specific methods not covered by groups G01N1/00 - G01N31/00
- G01N33/48—Biological material, e.g. blood, urine; Haemocytometers
- G01N33/50—Chemical analysis of biological material, e.g. blood, urine; Testing involving biospecific ligand binding methods; Immunological testing
- G01N33/72—Chemical analysis of biological material, e.g. blood, urine; Testing involving biospecific ligand binding methods; Immunological testing involving blood pigments, e.g. haemoglobin, bilirubin or other porphyrins; involving occult blood
-
- G—PHYSICS
- G01—MEASURING; TESTING
- G01N—INVESTIGATING OR ANALYSING MATERIALS BY DETERMINING THEIR CHEMICAL OR PHYSICAL PROPERTIES
- G01N21/00—Investigating or analysing materials by the use of optical means, i.e. using sub-millimetre waves, infrared, visible or ultraviolet light
- G01N21/17—Systems in which incident light is modified in accordance with the properties of the material investigated
- G01N21/25—Colour; Spectral properties, i.e. comparison of effect of material on the light at two or more different wavelengths or wavelength bands
- G01N21/31—Investigating relative effect of material at wavelengths characteristic of specific elements or molecules, e.g. atomic absorption spectrometry
- G01N21/314—Investigating relative effect of material at wavelengths characteristic of specific elements or molecules, e.g. atomic absorption spectrometry with comparison of measurements at specific and non-specific wavelengths
- G01N2021/3148—Investigating relative effect of material at wavelengths characteristic of specific elements or molecules, e.g. atomic absorption spectrometry with comparison of measurements at specific and non-specific wavelengths using three or more wavelengths
Definitions
- This invention relates to a method and apparatus to assess the optical transmittance of a sample of unaltered whole blood at multiple wavelengths to attain an accurate measurement of its total hemoglobin concentration, the concentration of bilirubin, and the concentrations of oxy-, deoxy-, carboxy-, met-, and sulfhemoglobin.
- characteristics include 1) the complex chemical mixture of as many as five individual hemoglobin species that are present in varying concentrations in a typical blood sample, and 2) the complex optical properties of whole blood that result from a combination of true optical absorbance by multiple light-absorbing compounds
- Loretz U.S. Patent 4,357,105 teaches a method whereby the hemoglobin is released from the red blood cells by the process of hemolysis, i.e. by disrupting the red blood cell membrane. Simultaneously, the various hemoglobin species are diluted by reagent solutions that convert them into a single chemical form, cyanmethemoglobin, the concentration of which is then measured spectrophotometrically by conventional
- Figure 1 presents a graph of the extinction
- Patent 3,972,614 Lundsgaard, U.S. Patent 4,997,769 to eliminate the light scattering by the red blood cells.
- the hemolyzed sample is then irradiated with at least one distinct wavelength for each of the three, four, or five hemoglobin species presumed to be present in the sample.
- the major obstacle to making optical measurements is the intense light scattering caused by the highly concentrated red blood cells, e.g. 5.4 X 10 6
- red blood cells in the sample aggregation and sedimentation of red blood cells in the sample, 3) the different hemoglobin concentrations inside the red blood cells that alter their refractive index, and 4) the size and shape of the red blood cells.
- the size and shape of the red blood cells differ from one animal species to another; they are also altered by disease states (e.g. sickle-cell anemia and
- Patent 4,997,769 teaches a method for dealing with the residual turbidity that remains after the hemolysis process, it would be advantageous to eliminate hemolysis completely and make spectrophotometric measurements directly in unaltered whole blood.
- the Applicants have found that the scattering of light by unaltered (unhemolyzed) whole blood differs in five crucial ways from the turbidity of hemolyzed blood.
- hemolyzed blood is insignificant in magnitude in
- red blood cells are not only a function of wavelength, but it also depends on the composition of the hemoglobin contained in the red blood cells, i.e. the light
- unpredictable light scattering include 1) the different plasma protein concentrations that determine the
- refractive index of plasma in one sample versus another 2) the aggregation of red blood cells in the sample, 3) the different hemoglobin concentrations inside the red blood cells that alter their refractive index, 4) the size and shape of the red blood cells, 5) chylomicrons or other light-scattering lipid particles, 6) cell
- Patent 4,134,678; Raffaele, U.S. Patent 4,013,417; and Johansen et al., U.S. Patent 3,972,614 would also fail to yield valid results on unhemolyzed whole blood because these methods also fail to capture the light scattered at large angles by the sample, and because their
- the present invention eliminates the need to hemolyze the blood sample and the need to chemically convert the various hemoglobin derivatives to a single species.
- the present invention makes appropriate measurements of the light scattering by red blood cells and of other light losses in unaltered, whole blood and then uses its assessment of these light losses to correct mathematically the measurements of total hemoglobin concentration and the concentrations of the individual hemoglobin species.
- the present invention avoids the problems caused by hemolysis such as the
- the present invention includes the following
- sulfhemoglobin 1.
- a spectrophotometric apparatus including an optical cuvette in which all optical parameters (for example, sample thickness, detector size and shape, sample-to-detector distance, wavelengths, monochromicity, and maximum angle of light capture by detector) are optimal values so as to minimize the contribution of light scattering to the total optical attenuation of unaltered whole blood and so as to maximize the optical parameters (for example, sample thickness, detector size and shape, sample-to-detector distance, wavelengths, monochromicity, and maximum angle of light capture by detector) are optimal values so as to minimize the contribution of light scattering to the total optical attenuation of unaltered whole blood and so as to maximize the
- a set of seven measuring wavelengths including the four selected by the aforementioned method; wherein the fifth wavelength is chosen specifically from the range of the visible spectrum in which absorption by bilirubin is especially large (475 to 500 nm); wherein the sixth wavelength is chosen specifically from the range of the visible spectrum in which absorption by sulfhemoglobin is especially large (615 to 625 nm); and wherein the seventh wavelength is chosen from that part of the spectrum where absorbance by bilirubin and each of the five hemoglobin species is as small as possible in comparison with the effects of light scattering, and small compared with the absorption by at least one of the pigments of interest at each of the other six
- the seventh wavelength the longest
- wavelength is preferably shorter than 675 nm to avoid errors due to the possible presence of indocyanine green dye in the sample and longer than 660 nm to avoid the relatively large absorbance of methemoglobin.
- concentration measurements for the effects of finite bandwidth of the substantially monochromatic measuring wavelengths wherein the errors due to finite bandwidth of the substantially monochromatic measuring wavelengths are treated as functions of the concentrations of oxy-, carboxy-, met-, deoxy-, and sulfhemoglobin present in each analyzed sample.
- Figure 1 is a graph of absorbance spectra for the five primary hemoglobin species.
- Figure 2 is a graph comparing the light scattering of unaltered whole blood with that of hemolyzed blood.
- Figure 3 is a graph of the theoretical wavelength dependence of the scattering of light by red blood cells.
- Figure 4 is a graph of the wavelength dependence of the light scattering by red blood cells in unaltered whole blood in the present invention for varying
- hemoglobin compositions of whole blood are hemoglobin compositions of whole blood.
- Figure 5 is a graph of the wavelength dependence of the nonspecific light-scattering losses in unaltered whole blood for varying hemoglobin compositions of whole blood.
- Figure 6 is a block diagram of the present invention including the optical geometry of the present invention.
- Figure 7 is a graph of the errors in the
- Figure 8 is a flow chart of the method in accordance with the present invention to select four principal measuring wavelengths.
- Figure 9 is a flow chart of a first method of operating the apparatus of Figure 6, in accordance with the present invention, to correct for light scattering.
- Figure 10 is a flow chart of a second method of operating the apparatus of Figure 6, in accordance with the present invention, to correct for light scattering.
- Figure 11a-e includes a graphical computer program listing of an embodiment of the method of Figure 8.
- Specific Scattering Factor Known factor causing light scattering, and thus light losses, in unaltered whole blood, the predominant example of which is light scattering due to red blood cells (RBCs). Other specific scattering factors include lipid particles, cell fragments, microscopic clots, and light-sieving effects of sedimented RBCs.
- Nonspecific Scattering Factor Unknown factor causing light scattering, and thus light losses in unaltered whole blood 3.
- Total Light-scattering Losses The sum of light losses due to light scattering by red blood cells, other known causes, and unknown causes. In other words, the sum of light losses due to Specific and Nonspecific
- Total Hemoglobin Concentration Sum of the amounts of the various hemoglobin species divided by the volume of blood, i.e., the total amount of hemoglobin in a mixture of oxy-, carboxy-, met-, deoxy-, and
- Error Index The sum of the absolute values of the errors that are induced in the measurement of the relative concentration of the given hemoglobin species (either oxy-, carboxy-, or methemoglobin) due to a 1% (relative) change in each of OD 1 ,...,OD 4 .
- Unaltered Whole Blood Whole blood that has been neither hemolyzed nor diluted.
- Figure 6 shows the presently preferred embodiment of the present invention which includes a digital computer 13; a computer-controlled light source 10 capable of sequentially emitting at least seven different
- the normal measurement cycle comprises 1) recording the dark current from the photodetector when the light source 10 is turned off, 2) recording the incident light intensity at each of the selected wavelengths, 3) placing a sample of
- all measurements are made at a substantially constant temperature.
- light source 10 may be a
- light source 10 may be a bank of light-emitting diodes (LED) arranged so that the emissions of each LED pass through a narrow-band optical interference filter before falling on the sample.
- light source 10 may be a white light source such as a halogen lamp optically coupled to a computer-controlled monochromator. In the first two embodiments, light source 10 may be pulsed at a frequency of
- Disposable cuvette 11 has a short optical path chosen to minimize total radiation scattering relative to absorbance by minimizing the number of scattering
- Cuvette 11 may have an optical pathlength of 80 to 150 ⁇ m. In one embodiment, the optical pathlength is 90 ⁇ 10 ⁇ m.
- Large-area radiation detector 12 is sensitive to the selected measuring radiation frequencies and may be placed within a distance d of from 0 to 10 mm, from cuvette 11.
- Detector 12 has a large active area and is placed close to cuvette 11 in order to capture radiation scattered at wide angles by the whole blood sample contained within cuvette 11.
- the distance d from cuvette 11 to detector 12 is no more than 1.0 mm
- the active area of detector 12 is at least 150 mm 2 , and preferably at least 600 mm 2
- the receiving half angle ⁇ of the detector 12, with respect to the point where the incident radiation impinges on the sample is at least 30° and preferably at least 70°.
- Digital computer 13 may be any type of programmable computer, for example, an Apple Macintosh computer. In order to render the apparatus as portable as possible, digital computer 13 may be a programmed microprocessor, such as one of the family of Motorola 68000
- configuration of the present invention is to maximize the true optical absorbance of unaltered whole blood and to minimize the effects of light scattering so that the apparent optical density of the sample measured by the detector is due primarily to absorbance with as small a contribution by light scattering as possible.
- the optical geometry presented above when used alone, does not attain commercially acceptable accuracy, i.e. it does not measure the
- the optical apparatus of the present invention achieves commercially acceptable accuracy when used in combination with the corrections (described below) that correct the hemoglobin concentration measurements for the effects of light scattering by the red blood cells, for nonspecific light-scattering losses, and for the effects of the finite spectral bandwidth of the plurality of substantially monochromatic wavelengths.
- wavelengths for HbO 2 , HbCO, Hi, Hb, SHb, and bilirubin Four principal wavelengths among the first six are chosen to measure HbO 2 , HbCO, Hi and Hb and are chosen to minimize the conversion factors by which errors in the optical density measurements (OD 1 ,...,OD 4 ) convert to errors in the measurements of %HbO 2 , %HbCO, and %Hi. The method for selecting these four wavelengths is described as follows.
- OD 1 ,...,OD 4 are defined as the absorbances of the hypothetical sample at the four wavelengths ⁇ 1 ,..., ⁇ 4 , thus
- %HbO 2 , %HbCO, %Hi, and %Hb are mathematical functions of OD 1 ,...,OD 4 as shown in the following equations:
- THb' indicates that SHb is left out of the sum.
- the derivatives e.g. d(%HbCO)/d(OD 3 ), are taken at the fixed values of OD 1 ,...,OD 4 determined for the fixed hypothetical sample whose hemoglobin is comprised of 85% HbO 2 and 15% Hb.
- An error criterion for the quadruple of wavelengths ⁇ 1 ,..., ⁇ 4 is then defined as the maximum of these three error indices.
- the mathematical criterion of the present invention consists in selecting the unique quadruple of wavelengths in the 510-630 nm range which minimizes the error criterion. The wavelengths are searched by 2 nm increments. When the extinction
- the final four wavelengths selected by this criteria are 518, 562, 580, and 590 nm.
- the Best Error Criterion is set to 10 10 , and the first quadruple of wavelengths is selected.
- the first quadruple may be 510, 512, 514, and 516 nm.
- Control then passes to block 82 where the Error Index for each of HbO 2 , HbCO, and Hi are computed. Then, control passes to block 83 where the Error Criterion is set to the absolute value of the Error Indices calculated in block 82.
- decision block 84 the Error Criterion calculated in block 83 is compared with the Best Error Criterion. If the Error Criterion is less than the Best Error Criterion, control passes to block 85 where the Best Error Criterion is set equal to the Error Criterion and the best quadruple of wavelengths is set equal to the present quadruple of wavelengths. Control then passes to block 86. If, on the other hand, decision block 84 determines that the Error Criterion is not less than the Best Error Criterion, control passes directly to decision block 86.
- decision block 86 it is determined whether the present quadruple of wavelengths is equal to the last quadruple of wavelengths, for example, 624, 626, 628 and 630 nm. If so, control passes to block 88 where the Best Error Criterion and best quadruple of wavelengths is reported. If, on the other hand, block 86 determines that the last quadruple has not been processed, control passes to block 87 where the next quadruple of wavelengths is formed, and control returns to block 82 for continued processing. To form the next quadruple, only one of the wavelengths at a time is changed by 2 nm. This procedure results in the analysis of all possible combinations of four wavelengths between 510 and 630 nm. Any set having duplicate wavelengths is discarded.
- Figures 11a-e hereto includes a source code listing in LabView graphical language which embodies the method of the flow chart of Figure 8.
- the method of Figure 8 either in the form of the source code of Figures 11a-e, or in an equivalent form, is used to program a computer to perform the wavelength quadruple selecting method of the present invention.
- a Scattering Factor is any specific or nonspecific cause of light scattering, i.e. any factor, known or unknown, that causes light scattering and hence light losses in unaltered whole blood. Examples are red blood cells, lipid particles, red blood cell aggregation, clotting, sedimentation, etc.
- n measuring wavelengths are employed to measure k constituent
- n - k extra equations provide a means by which errors due to n - k scattering factors can be compensated.
- Each specific scattering factor in the above definition is assumed to contribute in a well-defined way to the apparent
- OD 1 OD 1abs + OD 1y1 + . . . + OD 1yp
- OD 2 OD 2abs + OD 2y1 + . . . + OD 2yp
- OD n OD nabs + OD ny1 + . . . + OD nyp
- 1, ..., n wavelength indices
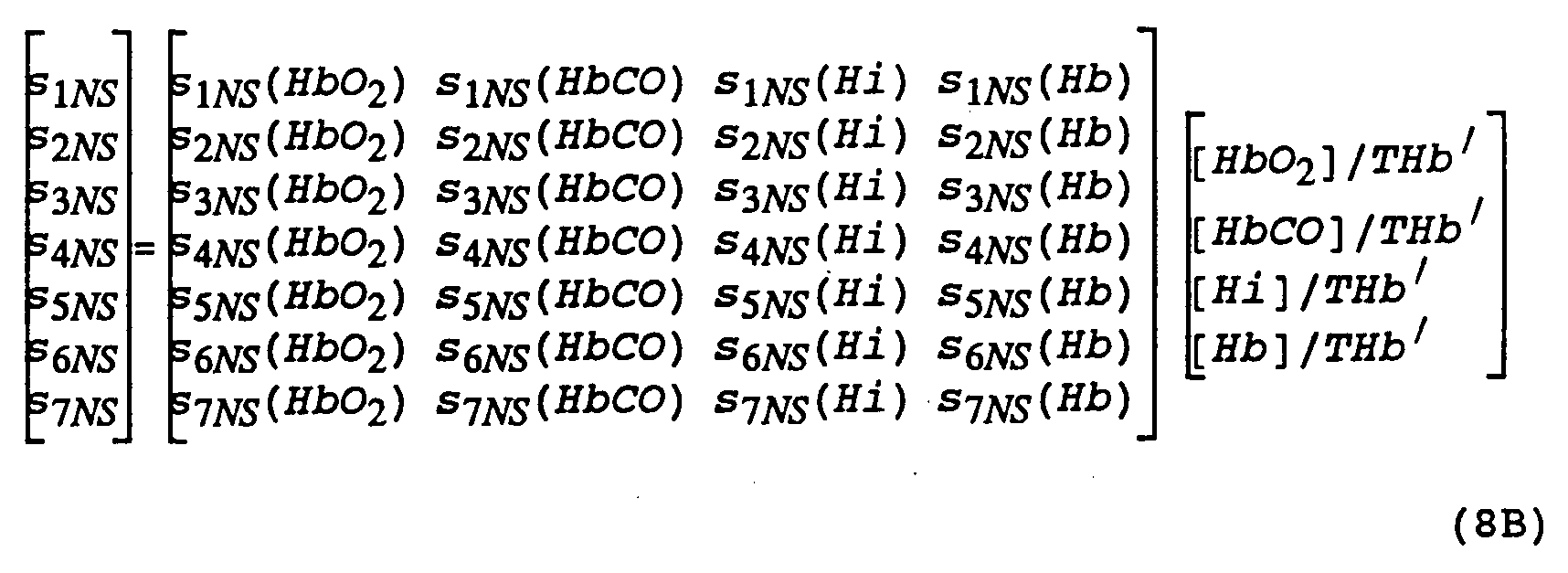
- the scattering vectors s yj vary with the hemoglobin species present in the sample under test.
- the scattering vectors s yj are different in completely oxygenated blood and blood completely saturated with carbon monoxide. Therefore, in the present invention, the scattering vectors s yj are described as functions of the concentrations of the hemoglobin species present in the sample under test.
- each scattering vector s yj depends on the hemoglobin species composition of the sample under test, one further distinguishes such scattering vectors as s yj (HbO 2 ), s yj (HbCO), etc.
- s yj HbO 2
- s yj HbCO
- h is the number of hemoglobin species present among the total number k of light-absorbing compounds
- X 1 , ..., x h denote the h hemoglobin species being measured.
- scattering factors have been identified: 1) light
- Embodiments A and B Disclosed are two embodiments of the corrections for light scattering: Embodiments A and B.
- Embodiment A the following rules hold: only light scattering by the red blood cells is considered (so the nonspecific
- Embodiment B the following rules hold: both light scattering by red blood cells and nonspecific light scattering are considered, and the concentrations of five compounds are measured, namely HbO 2 , HbCO, Hi, Hb and br.
- Both embodiments use the same set of seven wavelengths. As explained above, one wavelength (488 nm) is chosen at which absorbance by bilirubin is relatively large, another wavelength (622 nm) is chosen at which absorbance by sulfhemoglobin is relatively large, and another wavelength (672 nm) is used because light
- the mathematical criterion selected an optimal set of four wavelengths (522,562,584, and 600 nm) for measuring HbO 2 , HbCO, Hi with maximum accuracy. If the light source is either a battery of light-emitting diodes combined with optical interference filters or a white light source with a monochromator, these seven
- wavelengths can be used in either Embodiment A or B of the light-scattering corrections. However, if the samarium-neon hollow-cathode lamp is used, the most appropriate wavelengths among its emission lines are 488.4, 520.1, 562.4, 585.2, 597.5, 621.7, 671.7 nm.
- this set of wavelengths can be used in both Embodiments A and B of the light-scattering corrections.
- values for the extinction coefficients for bilirubin and the hemoglobin species can be determined. Therefore, the following equations obtain in Embodiments A and B of the light-scattering corrections.
- THB' [HBO 2 ] + [HbCO] + [Hi] + [Hb]
- THb [HbO 2 ] + [HbCO] + [Hi] + [Hb] + [SHb]
- THb' [HbO 2 ] + [HbCO] + [Hi] + [Hb].
- OD 1 , ..., OD 7 are the apparent optical densities of a sample of unaltered whole blood measured at each of the seven wavelengths, 488.4, 520.1, 562.4, 585.2, 597.5, 621.7, 671.7 nm, respectively.
- the method of finding the correct values for the scattering vectors SRBC and S NS when the relative concentrations (e.g., [HbO2]/THb) are initially unknown proceeds as follows.
- Default values for the scattering vectors S RBC and S NS are chosen to be the scattering vectors S RBc (HbO 2 ) and S NS (HbO 2 ), i.e. those values that are valid in case the sample is comprised purely of oxyhemoglobin.
- Embodiment A or m NSscat (Embodiment B) are computed.
- the initial hemoglobin and bilirubin concentrations are not yet accurate enough to report as final results, but they are sufficiently close to the true values to compute more accurate S RBC and S NS vectors for the given blood sample according to equation 7A or equations 7B and 8B.
- concentrations to compute more accurate S RBC or both S RBC and S NS vectors and in turn using the most recently computed S RBC or both S RBC and S NS vectors to compute more accurate hemoglobin and bilirubin concentrations provides an iterative scheme whereby the hemoglobin and bilirubin concentrations quickly converge to their final values.
- the fourth iteration of the computation of these concentrations is sufficiently accurate to report.
- Table I shows the values for the scattering vectors S RBC (HbO 2 ), S NS (HbO 2 ), S RBC (HbCO), S NS (HbCO), S RBC (Hb), and S NS (Hb), which the Applicants have measured and have found to be valid for both present Embodiments A and B of the light-scattering corrections.
- Figures 4 and 5 show the same data graphically at each of the measuring wavelengths (488.4, 520.1, 562.4, 585.2, 597.5, 621.7, and 671.7 nm).
- the present embodiment of the invention does not include measured values for the scattering vectors S RBC (Hi), S NS (Hi) or S RBC (SHb) because these less common hemoglobin species usually occur in low
- indices 1, ..., 7 refer to the seven wavelengths 488.4, 520.1, 562.4, 585.2, 597.5, 621.7, and 671.7 nm, respectively.
- the nonspecific scattering factor (NS) discovered by the Applicants provides a refinement of the more coarse correction for scattering by the red blood cells (RBC).
- RBC red blood cells
- a method is used to correct the measurements of the concentrations of HbO 2 , HbCO, Hi, Hb, SHb, and br for the effects of the finite bandwidth of the substantially monochromatic measuring wavelengths.
- This method is not necessary when the measuring wavelengths provided by light source B are sufficiently monochromatic, as is the case when the substantially monochromatic wavelengths are provided by isolated emission lines of a hollow cathode lamp.
- substantially monochromatic light is used, a range of (wavelength-dependent) extinction coefficients is
- the extinction coefficients of the hemoglobin species are linear functions of the concentrations of HbO 2 , HbCO, Hi, Hb, SHb, and bilirubin present in the sample under test, and the corrections in concentrations (given below) are linear functions of [HbO 2 ], [HbCO], [Hi], [Hb], [SHb], and Tbr.
- the order of operation of the invention should be first to measure the optical densities at each of the seven wavelengths, then to apply the corrections for light scattering by the red blood cells and for nonspecific light scattering losses, and finally to make the corrections for the finite spectral bandwidth of the light source.
- the method for the compensation of errors due the effects of the finite bandwidths of the substantially monochromatic wavelengths emitted by light source B proceeds as follows. After values for the concentrations have been corrected for the effects of light scattering by the red blood cells and for nonspecific light-scattering losses, the corrected concentration values, [HbO2], [HbCO], [Hi], [Hb], [SHb], and Tbr, are then used to compute spectral bandwidth corrections according to the following matrix equations:
- Control then returns to block 93. If, on the other hand, decision block 95 determines that counter n is greater than four, control passes to decision block 97 where it is determined whether the spectral width is greater than 1 nm. If so, control passes to block 98 where the finite bandwidth correction of equation 9A is performed. Then, in block 99, the latest values for the concentrations of the six constituent components are reported. If, on the other hand, decision block 97 determines that the
- Appendix A includes a source code listing in the C programming language which embodies the method of the flow chart of Figure 9.
- the method of the flow chart of Figure 9 embodied in the source code program of Appendix A or an equivalent program is used to program computer 13 of Figure 6, to cause the
- the counter n is initialized to zero. Then, in block 92, scattering vector s RBC is set equal to s RBC (HbO 2 ) and s NS is set equal to s NS (HbO 2 ). Then, in block 103 equation 6B is used to solve for
- control then returns to block 103. If, on the other hand, decision block 105 determines that counter n is greater than four, control passes to decision block 107 where it is determined whether the spectral width is greater than 1 nm. If so, control passes to block 108 where the finite bandwidth correction of equation 9B is performed. Then, in block 109, the latest values for the concentrations of the six constituent components are reported. If, on the other hand, decision block 107 determines that the spectral width is not greater than 1 nm, control passes directly to block 109 for report of the concentrations.
- Appendix B includes a source code listing in the C programming language which embodies the method of the flow chart of Figure 10.
- the method of the flow chart of Figure 10 embodied either in the source code program of Appendix B or an equivalent program, is used to program computer 13 of Figure 6, to cause the apparatus of Figure 6 to perform the method of Embodiment B to correct for light scattering.
- Embodiment C which utilizes one more
- Embodiment C uses the same first seven wavelengths as do Embodiments A and B. In Embodiment C, the following rules hold: both light scattering by red blood cells and nonspecific light scattering are
- the eighth wavelength is chosen so that the differences e 6HbO2 - e 8HbO2 , e 6HbCO - e 8HbCO , e 6Hi - e 8Hi , e 6Hb - e 8Hb , e 6br - e 8br , e 6RBC - e 8RBC , and e 6NS - e 8NS , are simultaneously small while e 6SHb - e 8SHb is quite large, i.e., in the 635 to 645 nm range.
- the choice of the eighth wavelength in view of the mathematical relationship between a matrix and its inverse, assures that the computation of sulfhemoglobin concentration is primarily dependent on the 6th and 8th wavelengths and is affected very little by the other six wavelengths.
- Embodiment C preferably uses 638 nm as its eighth
- the preferred eighth wavelength among its emission lines is 638.3 nm.
- OD 1 , ..., OD 8 are the apparent optical densities of a sample of unaltered whole blood measured at each of the eight wavelengths, 488.4, 520.1, 562.4, 585.2, 597.5, 621.7, 671.7, and 638.3 nm, respectively.
- the Radiometer OSM3 employs an ultrasonic hemolyzer, and is believed to embody the optical geometry of Johansen et al. (U.S. Patent
- the OSM3 In normal operation, the OSM3 first ultrasonically hemolyses each sample, then makes measurements of the sample's optical absorbance at multiple wavelengths, and finally uses the method of Lundsgaard to correct for the residual turbidity of the hemolyzed sample. To determine whether the method and apparatus of Lundsgaard could accurately measure hemoglobin concentrations in unaltered whole blood, the Applicants analyzed blood samples with the OSM3 operating normally and then analyzed the same blood samples with the OSM3's ultrasonic hemolyzer disabled.
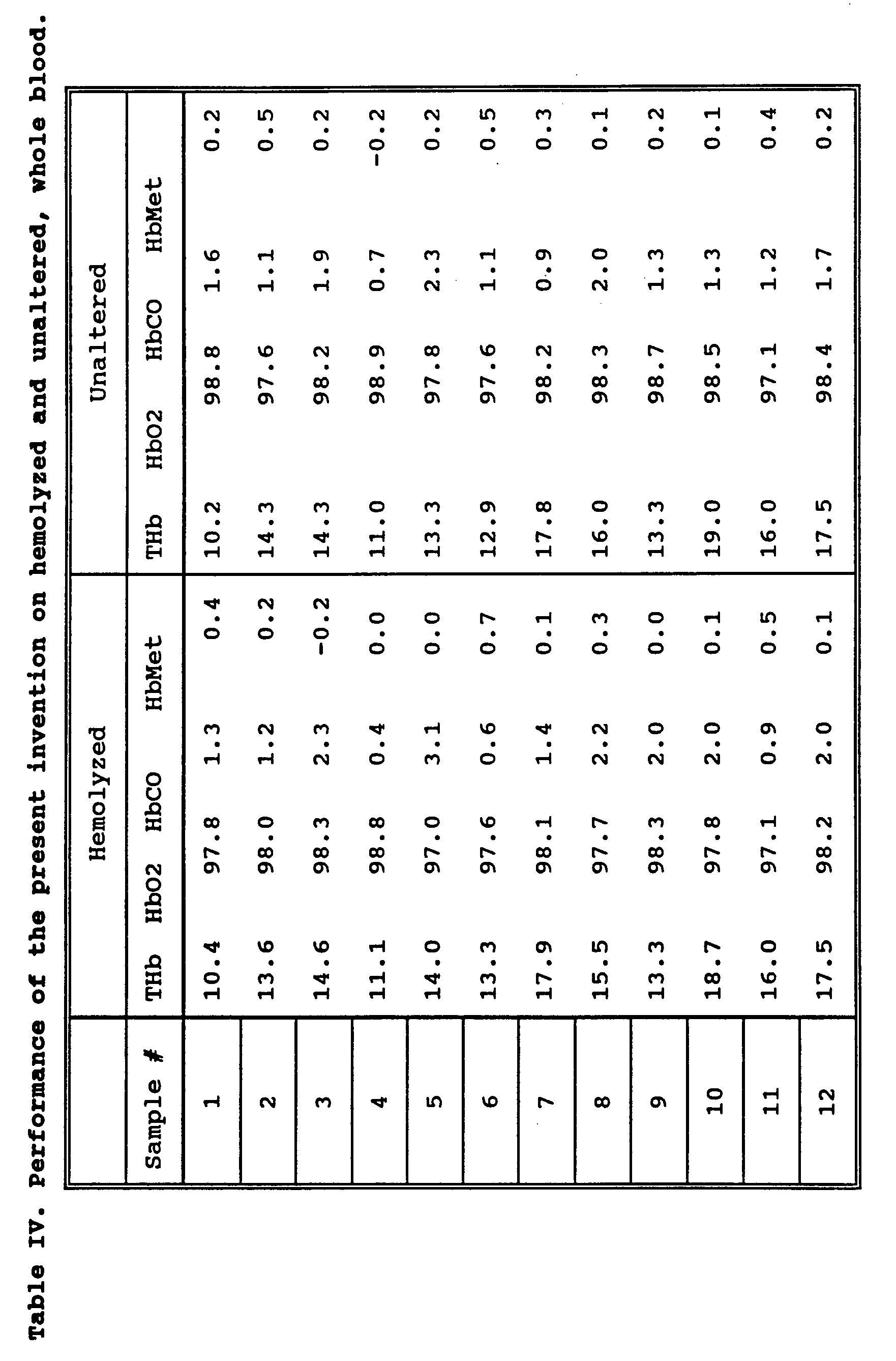
- Table III shows that the Radiometer OSM3, believed to use the method and apparatus of Lundsgaard (U.S.).
- Patent 4,997,769 gives completely erroneous results when the blood sample is not hemolyzed. For example, measurements of the total hemoglobin concentrations with and without hemolysis differ by as much as 7.4 grams/dl. Similarly, it is physically impossible for the relative concentration of oxyhemoglobin to be 400% or for the concentration of carboxyhemoglobin to be negative (-99%). Thus, it is readily apparent that the method and apparatus of Lundsgaard fail to yield even plausible results on unaltered, whole blood.
- Table IV shows that the measured total hemoglobin concentrations with and without hemolysis typically differ by only a few tenths of a gram/dl. Similarly, the measurements of the relative concentrations of oxy-, carboxy-, and methemoglobin are consistently in close agreement in all of the samples. In summary, the results shown in Tables III and IV demonstrate conclusively that the present invention enables one skilled in the art to make accurate measurements of the hemoglobin
- xtmp1 getXvalue((vector *)XODs,0);
- xtmp2 x_abs(xtmp1)
- xtmp3 xtmp1 /xtmp2;
- AtimesX((matrix *)Atmp3,(vector *)Xtmp1,(vector *)Xtmp2); /* may discard Atmp3 now */
- xsum Xsum(( vector *)Xtmp3)
- EnTHb enable_thb_slp */
- EnTHb enable_thb_slp */
- EnTHb enable_thb_slp */
- EnTHb enable_thb_slp */
- xtmp4 XY_inproduct((vector *)Xtmp3,(vector *)Xtmp6);
- xtmp7 xtmp1 * xtmp4;
- xtmp9 xtmp7 + xtmp 8;
- xtmp4 xtmp9 / xsum; /* xtmp4 gets compared to -1.0 */
- xtmp5 XY_inproduct((vector *)Xtmp3, (vector *)Xtmp7);
- xtmp6 XY_inproduct((vector *)Xtmp3, (vector *)Xtmp8);
- xtmp4 xtmp5 * xtmp9
- xtmp2 xtmp6 * xtmp1;
- xtmp3 xtmp4 + xtmp2;
- xtmp4 xsum + xtmp3;
- xsum Xsum((vector *)Xtmp3)
- xtmp1 xTHbc * xsum
- xtmp2 xtmp1 - (l_real) 13.5;
- xtmp2 getXvalue( (vector *)Xconc,6);
- xtmp3 getXvalue((vector *)Xtmp1,4)
- xtmp2 xtmp3 / xsum
- xtmp3 Xsum((vector *)Xtmp1)
- xtmp2 xTHbc * xtmp1;
- AtimesB ((matrix *)Atmp1, (matrix *)ACsats,(matrix *)Atmp2);
- xtmp1 getXvalue((vector *)XODs,0);
- xtmp2 x_abs(xtmp1)
- xtmp3 xtmp1 / xtmp2;
- AtimesX((matrix *)Atmp3,(vector *)Xtmp1,( vector *)Xtmp2); /* may discard Atmp3 now */
- xsum Xsum((vector *)Xtmp3)
- EnTHb enable_thb_slp */
- EnTHb enable_thb_slp */
- EnTHb enable_thb_slp */
- xtmp4 XY_inproduct((vector *)Xtmp3, (vector *)Xtmp6);
- xtmp7 xtmp1 * xtmp4;
- xtmp9 xtmp7 + xtmp 8;
- xtmp4 xtmp9 / xsum; /* xtmp4 gets compared to 1.25 */
- xtmp5 XY_inproduct((vector *)Xtmp3,(vector *)Xtmp7);
- xtmp6 XY_inproduct((vector *)Xtmp3, (vector *)Xtmp8);
- xtmp4 xtmp5 * xtmp9
- xtmp2 xtmp6 * xtmp1;
- xtmp3 xtmp4 + xtmp2;
- xtmp4 xsum + xtmp3;
- xsum Xsum((vector *)Xtmp3)
- xtmp1 xTHbc * xsum
- xtmp2 xtmp1 - (l_real)13.5;
- xtmp2 getXvalue((vector *)Xconc,6);
- xtmp3 getXvalue((vector *)Xtmp1,4)
- xtmp2 xtmp3 / xsum
- xtmp3 Xsum((vector *)Xtmp1)
- xtmp2 xTHbc * xtmp1;
Abstract
Description
Claims
Priority Applications (4)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| DE69328783T DE69328783T2 (en) | 1992-09-29 | 1993-09-27 | METHOD FOR DIRECT SPECTROPHOTOMETRIC MEASUREMENTS IN UNCHANGED BLOOD |
| AU51410/93A AU5141093A (en) | 1992-09-29 | 1993-09-27 | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood |
| EP93922402A EP0663070B1 (en) | 1992-09-29 | 1993-09-27 | Method for direct spectrophotometric measurements in unaltered whole blood |
| DK93922402T DK0663070T3 (en) | 1992-09-29 | 1993-09-27 | Method for direct spectrophotometric measurements in unchanged whole blood |
Applications Claiming Priority (2)
| Application Number | Priority Date | Filing Date | Title |
|---|---|---|---|
| US07/953,680 US6262798B1 (en) | 1992-09-29 | 1992-09-29 | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood |
| US07/953,680 | 1992-09-29 |
Publications (1)
| Publication Number | Publication Date |
|---|---|
| WO1994008237A1 true WO1994008237A1 (en) | 1994-04-14 |
Family
ID=25494388
Family Applications (1)
| Application Number | Title | Priority Date | Filing Date |
|---|---|---|---|
| PCT/US1993/009154 WO1994008237A1 (en) | 1992-09-29 | 1993-09-27 | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood |
Country Status (6)
| Country | Link |
|---|---|
| US (4) | US6262798B1 (en) |
| EP (1) | EP0663070B1 (en) |
| AU (1) | AU5141093A (en) |
| DE (1) | DE69328783T2 (en) |
| DK (1) | DK0663070T3 (en) |
| WO (1) | WO1994008237A1 (en) |
Cited By (7)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP0693682A2 (en) * | 1994-07-18 | 1996-01-24 | AVL Medical Instruments AG | Method for determining the concentration c of an absorbent homogeneously distributed on a support |
| EP0720013A3 (en) * | 1994-12-28 | 1997-09-10 | Coretech Medical Technologies | Spectrophotometric blood analysis |
| EP0800074A1 (en) * | 1996-04-02 | 1997-10-08 | AVL Medical Instruments AG | Apparatus and method for determining the concentration of hemoglobin derivatives in a nondiluted and nonhemolyzed whole blood sample |
| US5773301A (en) * | 1996-07-12 | 1998-06-30 | Avl Medical Instruments Ag | Method for optically determining total hemoglobin concentration |
| WO1999015880A1 (en) * | 1997-09-25 | 1999-04-01 | Bayer Corporation | Spectroscopic analysis of samples with turbidity and high absorbance |
| US6510330B1 (en) | 1998-11-30 | 2003-01-21 | Gambro Ab | Method and device for measuring blood parameters |
| US6943883B2 (en) | 2000-01-18 | 2005-09-13 | Radiometer Medical A/S | Apparatus, sample cuvette and method for optical measurements |
Families Citing this family (121)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US6262798B1 (en) * | 1992-09-29 | 2001-07-17 | Board Of Regents, The University Of Texas System | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood |
| EP1086366B1 (en) * | 1998-06-12 | 2010-04-14 | Radiometer Medical ApS | A method in quality control of a spectrophotometer |
| US6284142B1 (en) * | 1999-09-03 | 2001-09-04 | Baxter International Inc. | Sensing systems and methods for differentiating between different cellular blood species during extracorporeal blood separation or processing |
| US20030027347A1 (en) * | 2001-05-25 | 2003-02-06 | Phyllis Shapiro | Automated method for correcting blood analysis parameter results affected by interference from exogenous blood substitutes in whole blood, plasma, and serum |
| FR2829286B1 (en) * | 2001-09-03 | 2008-04-04 | Ge Med Sys Global Tech Co Llc | DEVICE AND METHOD FOR TRANSMITTING X-RAYS |
| US7050157B2 (en) | 2001-11-08 | 2006-05-23 | Optiscan Biomedical Corp. | Reagent-less whole-blood glucose meter |
| US6989891B2 (en) | 2001-11-08 | 2006-01-24 | Optiscan Biomedical Corporation | Device and method for in vitro determination of analyte concentrations within body fluids |
| US7061593B2 (en) | 2001-11-08 | 2006-06-13 | Optiscan Biomedical Corp. | Device and method for in vitro determination of analyte concentrations within body fluids |
| US6958809B2 (en) | 2001-11-08 | 2005-10-25 | Optiscan Biomedical Corporation | Reagent-less whole-blood glucose meter |
| WO2003045234A2 (en) * | 2001-11-21 | 2003-06-05 | Optiscan Biomedical Corporation | Method and apparatus for adjusting signal variation of an electronically controlled infrared transmissive window |
| US7009180B2 (en) * | 2001-12-14 | 2006-03-07 | Optiscan Biomedical Corp. | Pathlength-independent methods for optically determining material composition |
| US6862534B2 (en) * | 2001-12-14 | 2005-03-01 | Optiscan Biomedical Corporation | Method of determining an analyte concentration in a sample from an absorption spectrum |
| SE0104443D0 (en) * | 2001-12-28 | 2001-12-28 | Hemocue Ab | Analysis method and cuvette for that |
| US7002670B2 (en) * | 2002-06-12 | 2006-02-21 | Baxter International Inc. | Optical sensor and method for measuring concentration of a chemical constituent using its intrinsic optical absorbance |
| US20040132168A1 (en) * | 2003-01-06 | 2004-07-08 | Peter Rule | Sample element for reagentless whole blood glucose meter |
| EP1618389A1 (en) * | 2003-04-15 | 2006-01-25 | Optiscan Biomedical Corporation | Sample element qualification |
| US7271912B2 (en) * | 2003-04-15 | 2007-09-18 | Optiscan Biomedical Corporation | Method of determining analyte concentration in a sample using infrared transmission data |
| AU2004229538A1 (en) * | 2003-04-15 | 2004-10-28 | Optiscan Biomedical Corporation | Dual measurement analyte detection system |
| US9176121B2 (en) * | 2004-02-13 | 2015-11-03 | Roche Diagnostics Hematology, Inc. | Identification of blood elements using inverted microscopy |
| CA2460898A1 (en) * | 2004-03-09 | 2005-09-09 | James Samsoondar | Apparatus and method for combining in vivo and in vitro testing |
| WO2006040387A1 (en) * | 2004-10-11 | 2006-04-20 | Thermo Fisher Scientific Oy | Method for automatically detecting factors that disturb analysis by a photometer |
| EP1805499A4 (en) * | 2004-10-21 | 2010-07-21 | Optiscan Biomedical Corp | Method and apparatus for determining an analyte concentration in a sample having interferent |
| US8936755B2 (en) | 2005-03-02 | 2015-01-20 | Optiscan Biomedical Corporation | Bodily fluid composition analyzer with disposable cassette |
| US8251907B2 (en) | 2005-02-14 | 2012-08-28 | Optiscan Biomedical Corporation | System and method for determining a treatment dose for a patient |
| US20060200070A1 (en) * | 2005-02-14 | 2006-09-07 | Callicoat David N | Method and apparatus for calibrating an analyte detection system with a calibration sample |
| US20060189926A1 (en) * | 2005-02-14 | 2006-08-24 | Hall W D | Apparatus and methods for analyzing body fluid samples |
| US7860542B2 (en) * | 2005-02-14 | 2010-12-28 | Optiscan Biomedical Corporation | Analyte detection system with reduced sample volume |
| US7785258B2 (en) * | 2005-10-06 | 2010-08-31 | Optiscan Biomedical Corporation | System and method for determining a treatment dose for a patient |
| US8425444B2 (en) * | 2006-04-11 | 2013-04-23 | Optiscan Biomedical Corporation | Anti-clotting apparatus and methods for fluid handling system |
| US7364562B2 (en) * | 2005-10-06 | 2008-04-29 | Optiscan Biomedical Corp. | Anti-clotting apparatus and methods for fluid handling system |
| US20060194325A1 (en) * | 2005-02-14 | 2006-08-31 | Gable Jennifer H | Fluid handling cassette with a fluid control interface |
| SE530896C2 (en) * | 2005-04-01 | 2008-10-14 | Diaspect Medical Ab | Device for determining a blood hemoglobin concentration |
| US20100245803A1 (en) * | 2005-04-12 | 2010-09-30 | Chromedx Inc. | Blood sample holder for spectroscopic analysis |
| CA2517299A1 (en) * | 2005-08-26 | 2007-02-26 | Chromedx Inc. | Hollow needle assembly |
| US7740804B2 (en) * | 2005-04-12 | 2010-06-22 | Chromedx Inc. | Spectroscopic sample holder |
| US8206650B2 (en) * | 2005-04-12 | 2012-06-26 | Chromedx Inc. | Joint-diagnostic spectroscopic and biosensor meter |
| US20060228258A1 (en) * | 2005-04-12 | 2006-10-12 | Chromedx Inc. | Blood collection and measurement apparatus |
| CA2507323A1 (en) * | 2005-05-13 | 2006-11-13 | Chromedx Inc. | Diagnostic whole blood and plasma apparatus |
| US20060233667A1 (en) * | 2005-04-19 | 2006-10-19 | Chromedx Inc. | Joint-diagnostic spectroscopic and biosensor apparatus |
| US9561001B2 (en) | 2005-10-06 | 2017-02-07 | Optiscan Biomedical Corporation | Fluid handling cassette system for body fluid analyzer |
| US20080161723A1 (en) * | 2006-09-06 | 2008-07-03 | Optiscan Biomedical Corporation | Infusion flow interruption method and apparatus |
| US20070179436A1 (en) * | 2005-12-21 | 2007-08-02 | Braig James R | Analyte detection system with periodic sample draw and laboratory-grade analyzer |
| EP2645086A3 (en) * | 2006-03-16 | 2014-03-12 | Sysmex Corporation | Sample analyzer |
| SE530244C2 (en) * | 2006-05-05 | 2008-04-08 | Hemocue Ab | Method and system for quantitative hemoglobin determination |
| EP1987762A1 (en) * | 2007-05-03 | 2008-11-05 | F.Hoffmann-La Roche Ag | Oximeter |
| US20090160656A1 (en) * | 2007-10-11 | 2009-06-25 | Mahesh Seetharaman | Analyte monitoring system alarms |
| US8412293B2 (en) * | 2007-07-16 | 2013-04-02 | Optiscan Biomedical Corporation | Systems and methods for determining physiological parameters using measured analyte values |
| US20100145175A1 (en) * | 2008-08-22 | 2010-06-10 | Soldo Monnett H | Systems and methods for verification of sample integrity |
| US8597190B2 (en) | 2007-05-18 | 2013-12-03 | Optiscan Biomedical Corporation | Monitoring systems and methods with fast initialization |
| WO2008144575A2 (en) * | 2007-05-18 | 2008-11-27 | Optiscan Biomedical Corporation | Fluid injection and safety system |
| US8417311B2 (en) | 2008-09-12 | 2013-04-09 | Optiscan Biomedical Corporation | Fluid component analysis system and method for glucose monitoring and control |
| US7972296B2 (en) * | 2007-10-10 | 2011-07-05 | Optiscan Biomedical Corporation | Fluid component analysis system and method for glucose monitoring and control |
| KR100885123B1 (en) | 2007-08-31 | 2009-02-20 | 김세헌 | Portable bilirubin analyzer |
| WO2009048977A1 (en) * | 2007-10-08 | 2009-04-16 | Optiscan Biomedical Corporation | Low draw volume analyte detection systems |
| CA2702113A1 (en) * | 2007-10-11 | 2009-04-16 | Optiscan Biomedical Corporation | Synchronization and configuration of patient monitoring devices |
| US7959598B2 (en) | 2008-08-20 | 2011-06-14 | Asante Solutions, Inc. | Infusion pump systems and methods |
| US20100198037A1 (en) * | 2009-01-30 | 2010-08-05 | Cole Steven W | Feedback sensor for real-time management of sickle cell disease |
| US8970820B2 (en) | 2009-05-20 | 2015-03-03 | Nikon Corporation | Object exchange method, exposure method, carrier system, exposure apparatus, and device manufacturing method |
| EP2456355B1 (en) | 2009-07-20 | 2016-09-14 | Optiscan Biomedical Corporation | Adjustable connector and dead space reduction |
| US8731639B2 (en) | 2009-07-20 | 2014-05-20 | Optiscan Biomedical Corporation | Adjustable connector, improved fluid flow and reduced clotting risk |
| US9554742B2 (en) | 2009-07-20 | 2017-01-31 | Optiscan Biomedical Corporation | Fluid analysis system |
| US10475529B2 (en) | 2011-07-19 | 2019-11-12 | Optiscan Biomedical Corporation | Method and apparatus for analyte measurements using calibration sets |
| US8521244B2 (en) * | 2009-09-16 | 2013-08-27 | Analogic Corporation | Physiological parameter monitoring apparatus |
| ES2369686B1 (en) * | 2009-11-16 | 2012-12-04 | Alejandro Cáceres Gálvez | Portable equipment for measuring the concentration of hemoglobin derivatives in arterial blood in a non-destructive manner and use procedure |
| WO2011156522A1 (en) | 2010-06-09 | 2011-12-15 | Optiscan Biomedical Corporation | Measuring analytes in a fluid sample drawn from a patient |
| US8489164B2 (en) * | 2010-10-27 | 2013-07-16 | Medtronic, Inc. | Monitoring of tissue hemoglobin concentration |
| US9522396B2 (en) | 2010-12-29 | 2016-12-20 | S.D. Sight Diagnostics Ltd. | Apparatus and method for automatic detection of pathogens |
| EP2729784A4 (en) | 2011-07-06 | 2015-05-13 | Optiscan Biomedical Corp | Sample cell for fluid analysis system |
| CN103917870B (en) | 2011-11-16 | 2016-04-13 | 贝克顿·迪金森公司 | For detecting the method and system of the analysis thing in sample |
| CN106840812B (en) | 2011-12-29 | 2019-12-17 | 思迪赛特诊断有限公司 | Methods and systems for detecting pathogens in biological samples |
| KR101608684B1 (en) | 2012-04-13 | 2016-04-05 | 바디텍메드(주) | Device and method for measuring hemoglobin level from whole blood |
| JP5961482B2 (en) * | 2012-08-20 | 2016-08-02 | 株式会社日立ハイテクノロジーズ | Spectrophotometer |
| TW201410869A (en) * | 2012-09-10 | 2014-03-16 | Maestrogen Inc | Protein detection device |
| CN104755925B (en) | 2013-01-11 | 2017-06-23 | 贝克顿·迪金森公司 | The point-of-care of low cost determines device |
| CN109342282A (en) * | 2013-05-09 | 2019-02-15 | 艾博特健康公司 | The method and apparatus for determining the parameter in uncracked blood sample based on hemoglobin |
| WO2014188405A1 (en) | 2013-05-23 | 2014-11-27 | Parasight Ltd. | Method and system for imaging a cell sample |
| IL227276A0 (en) | 2013-07-01 | 2014-03-06 | Parasight Ltd | A method and system for preparing a monolayer of cells, particularly suitable for diagnosis |
| EP3039477B1 (en) | 2013-08-26 | 2021-10-20 | S.D. Sight Diagnostics Ltd. | Digital microscopy systems, methods and computer program products |
| CN113477149B (en) | 2013-11-06 | 2023-09-12 | 贝克顿·迪金森公司 | Microfluidic devices and methods of making and using the same |
| US10018640B2 (en) | 2013-11-13 | 2018-07-10 | Becton, Dickinson And Company | Optical imaging system and methods for using the same |
| WO2015095239A1 (en) | 2013-12-18 | 2015-06-25 | Optiscan Biomedical Corporation | Systems and methods for detecting leaks |
| GB2523989B (en) | 2014-01-30 | 2020-07-29 | Insulet Netherlands B V | Therapeutic product delivery system and method of pairing |
| KR20170010361A (en) | 2014-05-31 | 2017-01-31 | 크로메드엑스 코포레이션 | Joint spectroscopic and biosensor system for point-of-care testing |
| US10482595B2 (en) | 2014-08-27 | 2019-11-19 | S.D. Sight Diagnostics Ltd. | System and method for calculating focus variation for a digital microscope |
| EP3094252B1 (en) | 2014-10-14 | 2021-08-25 | Becton, Dickinson and Company | Blood sample management using open cell foam |
| EP4261523A3 (en) | 2014-10-14 | 2023-12-06 | Becton, Dickinson and Company | Blood sample management using open cell foam |
| US9833557B2 (en) | 2014-12-19 | 2017-12-05 | Fenwal, Inc. | Systems and methods for determining free plasma hemoglobin |
| WO2016134137A1 (en) | 2015-02-18 | 2016-08-25 | Insulet Corporation | Fluid delivery and infusion devices, and methods of use thereof |
| JP6426832B2 (en) | 2015-03-10 | 2018-11-21 | ベクトン・ディキンソン・アンド・カンパニーBecton, Dickinson And Company | Microsample management system for biological fluid |
| WO2017040650A1 (en) | 2015-09-01 | 2017-03-09 | Becton, Dickinson And Company | Depth filtration device for separating specimen phases |
| JP6952683B2 (en) | 2015-09-17 | 2021-10-20 | エス.ディー.サイト ダイアグノスティクス リミテッド | Methods and devices for detecting entities in body samples |
| TWI584786B (en) | 2015-10-01 | 2017-06-01 | 緯創資通股份有限公司 | Method for sensing physiological feature |
| WO2017123525A1 (en) | 2016-01-13 | 2017-07-20 | Bigfoot Biomedical, Inc. | User interface for diabetes management system |
| CA3009351A1 (en) | 2016-01-14 | 2017-07-20 | Bigfoot Biomedical, Inc. | Adjusting insulin delivery rates |
| US11733150B2 (en) | 2016-03-30 | 2023-08-22 | S.D. Sight Diagnostics Ltd. | Distinguishing between blood sample components |
| US9976946B2 (en) | 2016-04-21 | 2018-05-22 | Instrumentation Laboratory Company | Optical flow cell and test head apparatus |
| US10288556B2 (en) | 2016-04-21 | 2019-05-14 | Instrumentation Laboratory Company | Optical flow cell apparatus and method for reducing deflection of sample chamber |
| EP3455607B1 (en) | 2016-05-11 | 2022-07-20 | Nova Biomedical Corporation | Whole blood so2 sensor |
| WO2017195205A1 (en) | 2016-05-11 | 2017-11-16 | S.D. Sight Diagnostics Ltd | Sample carrier for optical measurements |
| AU2017263807B2 (en) | 2016-05-11 | 2023-02-02 | S.D. Sight Diagnostics Ltd | Performing optical measurements on a sample |
| CA3031081C (en) | 2016-07-18 | 2021-08-31 | Siemens Healthcare Diagnostics Inc. | System and method for optical whole blood hemolysis detection |
| US10765807B2 (en) | 2016-09-23 | 2020-09-08 | Insulet Corporation | Fluid delivery device with sensor |
| US11921272B2 (en) | 2017-11-14 | 2024-03-05 | S.D. Sight Diagnostics Ltd. | Sample carrier for optical measurements |
| USD928199S1 (en) | 2018-04-02 | 2021-08-17 | Bigfoot Biomedical, Inc. | Medication delivery device with icons |
| CN112236826A (en) | 2018-05-04 | 2021-01-15 | 英赛罗公司 | Safety constraints for drug delivery systems based on control algorithms |
| US11628251B2 (en) | 2018-09-28 | 2023-04-18 | Insulet Corporation | Activity mode for artificial pancreas system |
| WO2020077223A1 (en) | 2018-10-11 | 2020-04-16 | Insulet Corporation | Event detection for drug delivery system |
| US10883927B2 (en) * | 2019-06-05 | 2021-01-05 | Taiwan Redeye Biomedical Inc. | Hemoglobin detecting device |
| US11801344B2 (en) | 2019-09-13 | 2023-10-31 | Insulet Corporation | Blood glucose rate of change modulation of meal and correction insulin bolus quantity |
| US11935637B2 (en) | 2019-09-27 | 2024-03-19 | Insulet Corporation | Onboarding and total daily insulin adaptivity |
| US11833329B2 (en) | 2019-12-20 | 2023-12-05 | Insulet Corporation | Techniques for improved automatic drug delivery performance using delivery tendencies from past delivery history and use patterns |
| US11551802B2 (en) | 2020-02-11 | 2023-01-10 | Insulet Corporation | Early meal detection and calorie intake detection |
| US11547800B2 (en) | 2020-02-12 | 2023-01-10 | Insulet Corporation | User parameter dependent cost function for personalized reduction of hypoglycemia and/or hyperglycemia in a closed loop artificial pancreas system |
| US11324889B2 (en) | 2020-02-14 | 2022-05-10 | Insulet Corporation | Compensation for missing readings from a glucose monitor in an automated insulin delivery system |
| DE102020104266B3 (en) * | 2020-02-18 | 2021-04-22 | Technische Hochschule Lübeck | Device and method for analyzing blood |
| US11607493B2 (en) | 2020-04-06 | 2023-03-21 | Insulet Corporation | Initial total daily insulin setting for user onboarding |
| US11684716B2 (en) | 2020-07-31 | 2023-06-27 | Insulet Corporation | Techniques to reduce risk of occlusions in drug delivery systems |
| US11904140B2 (en) | 2021-03-10 | 2024-02-20 | Insulet Corporation | Adaptable asymmetric medicament cost component in a control system for medicament delivery |
| DE102021116189A1 (en) | 2021-06-23 | 2022-12-29 | Benjamin Kern | Spectroscopy device and method for determining blood parameters |
| US11738144B2 (en) | 2021-09-27 | 2023-08-29 | Insulet Corporation | Techniques enabling adaptation of parameters in aid systems by user input |
| US11439754B1 (en) | 2021-12-01 | 2022-09-13 | Insulet Corporation | Optimizing embedded formulations for drug delivery |
Family Cites Families (33)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| US2878715A (en) | 1956-02-06 | 1959-03-24 | Mark C Rhees | Method of blood plasma prothrombin time determinations |
| US3296922A (en) | 1963-04-22 | 1967-01-10 | American Optical Corp | Apparatus for determining oxygen saturation of blood |
| US3516746A (en) | 1965-01-28 | 1970-06-23 | Shimadzu Corp | Cross slide spectrophotometer with a diffusing element between sample cell and photoelectric tube |
| US3527542A (en) | 1966-06-15 | 1970-09-08 | Beckman Instruments Inc | Cardiac output apparatus |
| US3638640A (en) | 1967-11-01 | 1972-02-01 | Robert F Shaw | Oximeter and method for in vivo determination of oxygen saturation in blood using three or more different wavelengths |
| US3649204A (en) | 1968-09-18 | 1972-03-14 | Farr Devices Inc | Metering pump for analytical samples |
| HU164637B (en) | 1970-02-02 | 1974-03-28 | ||
| US3799672A (en) | 1972-09-15 | 1974-03-26 | Us Health Education & Welfare | Oximeter for monitoring oxygen saturation in blood |
| GB1486505A (en) | 1974-06-04 | 1977-09-21 | Compur Werk Gmbh & Co | Handheld photoelectric appliance for testing liquids |
| US3972614A (en) | 1974-07-10 | 1976-08-03 | Radiometer A/S | Method and apparatus for measuring one or more constituents of a blood sample |
| IT1019866B (en) | 1974-08-09 | 1977-11-30 | Biomedix Ag | EQUIPMENT FOR THE DETERMINATION OF THE CONCENTRATION OF HEMOGLOBES NA TOTAL OXYGEN AND RISOTTA CAR BOSSIHEMOGLOBIN OF THE CAPACITY OF THE HEMOGLOBIN FOR THE OXYGEN OF THE SATURATION PER CENTUAL IN OXYGEN AND IN OXIDE OF CARBON IN SOLOIL OR BLOOD |
| US3922598A (en) | 1974-08-15 | 1975-11-25 | Robert R Steuer | Hematocrit measurements by electrical conductivity |
| CH581836A5 (en) | 1974-08-20 | 1976-11-15 | Contraves Ag | |
| US4057394A (en) | 1976-05-24 | 1977-11-08 | Miles Laboratories, Inc. | Test device and method for determining blood hemoglobin |
| DK146287C (en) | 1976-10-18 | 1984-01-30 | Radiometer As | PROCEDURE FOR DEOXYGENATION OF A BLOOD SAMPLING MATERIAL AND CAPILLAR BEARS USED BY THE PROCEDURE |
| US4134678A (en) | 1977-03-16 | 1979-01-16 | Instrumentation Laboratory Inc. | Automatic blood analysis apparatus and method |
| AT374008B (en) | 1977-10-25 | 1984-03-12 | Compur Electronic Gmbh | CUEVETTE |
| US4243883A (en) | 1979-01-19 | 1981-01-06 | Midwest Cardiovascular Institute Foundation | Blood hematocrit monitoring system |
| US4301412A (en) | 1979-10-29 | 1981-11-17 | United States Surgical Corporation | Liquid conductivity measuring system and sample cards therefor |
| US4303887A (en) | 1979-10-29 | 1981-12-01 | United States Surgical Corporation | Electrical liquid conductivity measuring system |
| US4502786A (en) | 1979-12-26 | 1985-03-05 | Helena Laboratories Corporation | Method and apparatus for automated determination of hemoglobin species |
| US4324556A (en) | 1980-03-25 | 1982-04-13 | The United States Of America As Represented By The Secretary Of The Navy | Portable COHB analyzer |
| US4453266A (en) | 1980-04-21 | 1984-06-05 | Rush-Presbyterian-St. Luke's Medical Center | Method and apparatus for measuring mean cell volume of red blood cells |
| US4357105A (en) | 1980-08-06 | 1982-11-02 | Buffalo Medical Specialties Mfg., Inc. | Blood diagnostic spectrophotometer |
| US4444498A (en) | 1981-02-27 | 1984-04-24 | Bentley Laboratories | Apparatus and method for measuring blood oxygen saturation |
| FR2530029A1 (en) | 1982-07-06 | 1984-01-13 | Centre Nat Rech Scient | IMPROVED LASER NEPHELOMETER FOR DETECTION OF ANTIGENS AND ANTIBODIES |
| US4700708A (en) | 1982-09-02 | 1987-10-20 | Nellcor Incorporated | Calibrated optical oximeter probe |
| US4565448A (en) | 1983-03-11 | 1986-01-21 | E. I. Du Pont De Nemours And Company | Particle counting apparatus |
| US4651741A (en) | 1985-05-30 | 1987-03-24 | Baxter Travenol Laboratories, Inc. | Method and apparatus for determining oxygen saturation in vivo |
| DK282085D0 (en) | 1985-06-21 | 1985-06-21 | Radiometer As | METHOD AND APPARATUS FOR DETERMINING BLOOD COMPONENTS |
| US4805623A (en) * | 1987-09-04 | 1989-02-21 | Vander Corporation | Spectrophotometric method for quantitatively determining the concentration of a dilute component in a light- or other radiation-scattering environment |
| US6262798B1 (en) * | 1992-09-29 | 2001-07-17 | Board Of Regents, The University Of Texas System | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood |
| US5064282A (en) * | 1989-09-26 | 1991-11-12 | Artel, Inc. | Photometric apparatus and method for measuring hemoglobin |
-
1992
- 1992-09-29 US US07/953,680 patent/US6262798B1/en not_active Expired - Lifetime
-
1993
- 1993-09-27 WO PCT/US1993/009154 patent/WO1994008237A1/en active IP Right Grant
- 1993-09-27 DK DK93922402T patent/DK0663070T3/en active
- 1993-09-27 DE DE69328783T patent/DE69328783T2/en not_active Expired - Lifetime
- 1993-09-27 EP EP93922402A patent/EP0663070B1/en not_active Expired - Lifetime
- 1993-09-27 AU AU51410/93A patent/AU5141093A/en not_active Abandoned
-
2001
- 2001-07-10 US US09/902,823 patent/US6519025B2/en not_active Expired - Fee Related
-
2002
- 2002-12-06 US US10/313,220 patent/US7075628B2/en not_active Expired - Fee Related
-
2006
- 2006-02-22 US US11/359,924 patent/US20060203225A1/en not_active Abandoned
Non-Patent Citations (2)
| Title |
|---|
| Phys. Med. Bio., Vol. 12, No. 2, 1967, ANDERSON et al., "Light Absorbing and Scattering Properties of Non-Haemolysed Blood", pages 173-184; see entire document. * |
| See also references of EP0663070A4 * |
Cited By (11)
| Publication number | Priority date | Publication date | Assignee | Title |
|---|---|---|---|---|
| EP0693682A2 (en) * | 1994-07-18 | 1996-01-24 | AVL Medical Instruments AG | Method for determining the concentration c of an absorbent homogeneously distributed on a support |
| EP0693682A3 (en) * | 1994-07-18 | 1996-10-30 | Avl Medical Instr Ag | Method for determining the concentration c of an absorbent homogeneously distributed on a support |
| EP0720013A3 (en) * | 1994-12-28 | 1997-09-10 | Coretech Medical Technologies | Spectrophotometric blood analysis |
| EP0800074A1 (en) * | 1996-04-02 | 1997-10-08 | AVL Medical Instruments AG | Apparatus and method for determining the concentration of hemoglobin derivatives in a nondiluted and nonhemolyzed whole blood sample |
| AT403412B (en) * | 1996-04-02 | 1998-02-25 | Avl Verbrennungskraft Messtech | DEVICE AND METHOD FOR DETERMINING THE CONCENTRATION OF HEMOGLOBIN DERIVATIVES IN AN UNDILINED, UNHEMOLYZED WHOLE BLOOD SAMPLE |
| US5773301A (en) * | 1996-07-12 | 1998-06-30 | Avl Medical Instruments Ag | Method for optically determining total hemoglobin concentration |
| WO1999015880A1 (en) * | 1997-09-25 | 1999-04-01 | Bayer Corporation | Spectroscopic analysis of samples with turbidity and high absorbance |
| US6172744B1 (en) | 1997-09-25 | 2001-01-09 | Bayer Corporation | Method and apparatus for performing spectroscopic analysis with applicability to samples with turbidity and absorption |
| US6219132B1 (en) | 1997-09-25 | 2001-04-17 | Bayer Corporation | Method and apparatus for performing spectroscopic analysis with applicability to samples with turbidity and absorption |
| US6510330B1 (en) | 1998-11-30 | 2003-01-21 | Gambro Ab | Method and device for measuring blood parameters |
| US6943883B2 (en) | 2000-01-18 | 2005-09-13 | Radiometer Medical A/S | Apparatus, sample cuvette and method for optical measurements |
Also Published As
| Publication number | Publication date |
|---|---|
| US20030202170A1 (en) | 2003-10-30 |
| US20060203225A1 (en) | 2006-09-14 |
| US6262798B1 (en) | 2001-07-17 |
| EP0663070A1 (en) | 1995-07-19 |
| US6519025B2 (en) | 2003-02-11 |
| US20020041371A1 (en) | 2002-04-11 |
| US7075628B2 (en) | 2006-07-11 |
| AU5141093A (en) | 1994-04-26 |
| DE69328783D1 (en) | 2000-07-06 |
| DE69328783T2 (en) | 2000-09-21 |
| DK0663070T3 (en) | 2000-10-02 |
| EP0663070A4 (en) | 1995-08-30 |
| EP0663070B1 (en) | 2000-05-31 |
Similar Documents
| Publication | Publication Date | Title |
|---|---|---|
| US6519025B2 (en) | Method and apparatus for direct spectrophotometric measurements in unaltered whole blood | |
| EP0419223B1 (en) | Characterizing biological matter in a dynamic condition using near infrared spectroscopy | |
| EP2016390B1 (en) | A method and a system for quantitative hemoglobin determination | |
| CA2468513C (en) | Analysis method and system therefor | |
| US5706208A (en) | Method for the prediction of properties of biological matter by analysis of the near-infrared spectrum thereof | |
| Zwart et al. | Multicomponent analysis of hemoglobin derivatives with reversed-optics spectrophotometer. | |
| CA2025329C (en) | Characterizing matter of biological origin using near infrared spectroscopy | |
| Polanyi et al. | New reflection oximeter | |
| Cookson et al. | A simple spectrophotometric method for the quantification of residual haemoglobin in platelet concentrates | |
| US20050037505A1 (en) | Spectroscopic method and apparatus for analyte measurement | |
| US7449339B2 (en) | Spectroscopic method and apparatus for total hemoglobin measurement | |
| Lin et al. | Detection of free hemoglobin in blood products using transmission spectra and fluorescence spectra for quality assurance | |
| US6623972B2 (en) | Automated method for detecting, quantifying and monitoring exogenous hemoglobin in whole blood, plasma and serum | |
| US6995835B2 (en) | Method and apparatus for measuring analytes in blood bags | |
| Anderson et al. | Studies on the light transmission of nonhemolyzed whole blood. Determination of oxygen saturation | |
| JP2005274568A (en) | Spectroscopic method and apparatus for total hemoglobin measurement | |
| US5939327A (en) | Measurement of bile pigments in serum or plasma | |
| US20050134833A1 (en) | Method and apparatus for measuring cell-by-cell hemoglobin | |
| Can et al. | Modeling diffuse reflectance spectra of donated blood with their hematological parameters | |
| US20240060957A1 (en) | Point-of-care testing system, analyzer and method | |
| RU2140083C1 (en) | Method of determination of content of main derivatives of hemoglobin | |
| Hallemann et al. | Technical aspects of bilirubin determination in whole blood | |
| Mullins et al. | Effects of Fluosol-DA (artificial blood) on clinical chemistry tests and instruments |
Legal Events
| Date | Code | Title | Description |
|---|---|---|---|
| AK | Designated states |
Kind code of ref document: A1 Designated state(s): AT AU BB BG BR BY CA CH CZ DE DK ES FI GB HU JP KP KR KZ LK LU LV MG MN MW NL NO NZ PL PT RO RU SD SE SK UA VN |
|
| AL | Designated countries for regional patents |
Kind code of ref document: A1 Designated state(s): AT BE CH DE DK ES FR GB GR IE IT LU MC NL PT SE BF BJ CF CG CI CM GA GN ML MR NE SN TD TG |
|
| DFPE | Request for preliminary examination filed prior to expiration of 19th month from priority date (pct application filed before 20040101) | ||
| 121 | Ep: the epo has been informed by wipo that ep was designated in this application | ||
| WWE | Wipo information: entry into national phase |
Ref document number: 1993922402 Country of ref document: EP |
|
| WWP | Wipo information: published in national office |
Ref document number: 1993922402 Country of ref document: EP |
|
| REG | Reference to national code |
Ref country code: DE Ref legal event code: 8642 |
|
| NENP | Non-entry into the national phase |
Ref country code: CA |
|
| WWG | Wipo information: grant in national office |
Ref document number: 1993922402 Country of ref document: EP |